Glaucoma
Glaucoma refers to a variety of diseases that share a common endpoint – Progressive damage to the optic nerve that results in loss of peripheral vision.
Aqueous fluid is created behind the iris at the ciliary body and circulates through the pupil to bring nutrients to the lens and cornea. It is then reabsorbed through small openings in the area where the cornea, lens and iris meet (the “angle”).
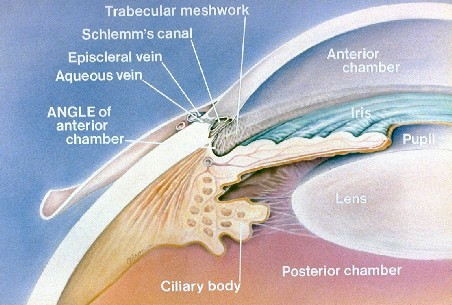
In Open-Angle Glaucoma, the most common type, fluid is made faster than it can be reabsorbed leading to increased pressure in the eye. The excess pressure causes the small nerve fibers that make up the optic nerve to be compressed, and over time, can cause irreparable damage. Changes in the optic nerve are seen first, followed by loss of peripheral vision in a variety of patterns. If left untreated, tunnel vision and eventually blindness will occur.
Known major risk factors for open-angle glaucoma include:
- Age
- Family History
- African descent
- Increased eye pressure
- Thin corneas
Previously, it was thought that glaucoma was a disease of increased pressure inside the eye. However, many patients with high eye pressures never develop glaucoma and conversely, many patients with “normal” pressures do develop glaucoma. Glaucoma is a slowly progressive disease in which changes may occur over many years, making it a difficult disease to diagnose. Because of this, we follow a number of patients as “Glaucoma Suspects”. These patients have risk factors for glaucoma or have an unusual appearance to the optic nerve that may be suggestive of glaucoma. A complete eye exam is the only way to detect the presence of glaucoma. The exam may include:
- Measurement of intraocular pressure (tonometry)
- Measurement of corneal thickness (pachymetry)
- Inspection of the angle (gonioscopy)
- Dilated examination of the optic nerve
- Laser measurements of the optic nerve for serial comparison (GDx, OCT, HRT)
- Formal visual field evaluation (perimetry)
Treatment of glaucoma is focused on lowering the pressure inside the eye. Prescription eyedrops are the initial treatment in all patients, and depending on the response, may be all that is required. In cases where medications alone are not sufficient, laser treatment (laser trabeculoplasty) can be done. If all else fails, surgery to relieve the pressure in the eye may be required (trabulectomy or tube shunt).
In Closed-Angle Glaucoma, the drain of the eye closes intermittently, leading to episodes of greatly increased pressure in the eye. In between episodes, eye pressure can be normal. This type of glaucoma usually occurs because of the anatomic configuration of the structures in the eye. This type of glaucoma can be cured by an in-office laser procedure to create a secondary drainage pathway for aqueous fluid.
Secondary Glaucoma is glaucoma caused by another disease process.
Pigment dispersion syndrome is a condition in which increased amounts of pigment circulate within the front portion of the eye. This often results in having pigment layered on the back of the cornea, thinning of the iris, and clogging of the ocular drainage system with pigment. This pigment can block the drainage channel enough to cause an increase in intraocular pressure (IOP). In cases of pigmentary glaucoma, the IOP often is very high, reaching levels above 40 mm Hg. Pigmentary dispersion leads to damage from glaucoma in 20% to 50% of patients. It is more common in males and often appears in people under 50 years of age.
Pseudoexfoliation syndrome is a relatively common disease that occurs in the eyes. It is marked by a dust-like material that is observed inside the eye on the surface of the iris and lens. In a small percentage of patients with pseudoexfoliation syndrome, the material can break away from the surface of the lens and become lodged in the the ocular drainage system, increasing intraocular pressure (IOP). This is referred to as pseudoexfoliation glaucoma. It can occur in one or both eyes and is most commonly seen in patients over the age of 70. Pseudoexfoliation glaucoma is found in all ethnic groups, but it is most commonly seen in people of Scandinavian ancestry. Treatment is often required for pseudoexfoliation glaucoma, consisting of medication, laser treatment, or surgery. Pseudoexfoliation can cause increased complications with cataract surgery. With proper treatment and monitoring, patients with pseudoexfoliation glaucoma tend to do well. Early diagnosis is important. Treatment is the same as for other forms of open-angle glaucoma, including medications, laser therapy, or surgery. With adequate treatment, the prognosis for pigmentary glaucoma is good.